Living with vascular dementia is challenging. But, even less discussed is the issue of caring for people who are living through the seven stages of vascular dementia.
Families and friends who know are caring for an individual with vascular dementia: we understand that living with and caring for someone with vascular dementia is tough. The progression of the condition differs for each individual, which means a one-size-fits-all approach won’t work for all.
And with the lifecycle of the disease differing for each person, being prepared to help loved ones can feel more like a burden than a privilege.
We get it, and we’re here to help.
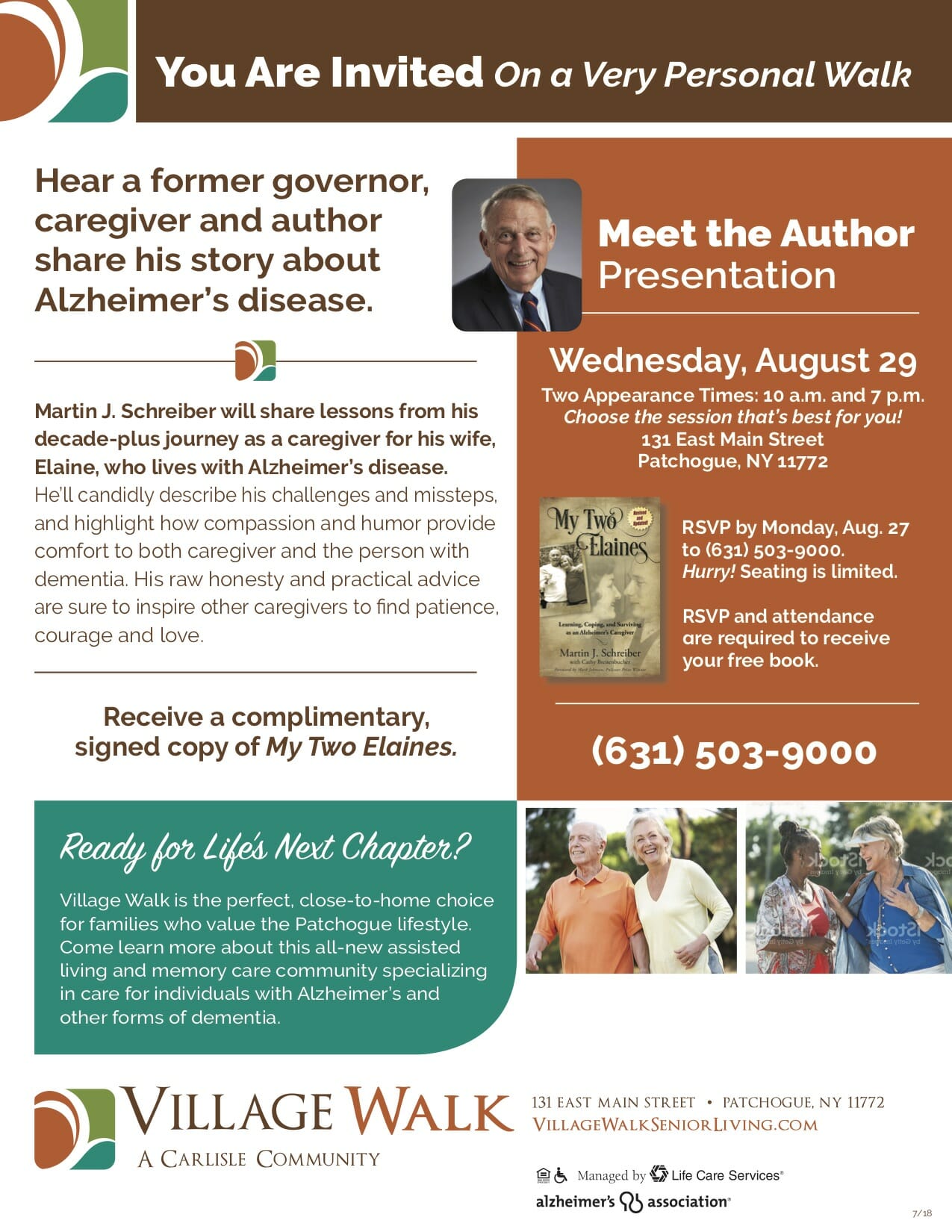
For more than 30 years, the expert caregivers and senior living team at Village Walk have been providing assisted living and memory care solutions for individuals, families, and friends living with vascular dementia.
If you’re wondering what to expect at each of the seven stages of vascular dementia, you’re not alone. Join us! We’ll lighten your load by providing helpful information about what to expect at each of the seven stages of vascular dementia.
Defining vascular dementia: what is it?
Before we dive into the specifics of stages of vascular dementia, we need to understand what vascular dementia is. Vascular dementia is a form of dementia similar to Alzheimer’s disease or Lewy body dementia.
Vascular dementia is caused by impaired blood flow to the brain, usually from a stroke or mini-stroke (also known as a transient ischemic attack (TIA)). When the lack of blood flow causes brain damage, vascular dementia can occur.
Since the prevalence of strokes among the 60-year and older community nearly doubles by the time a person hits 80 years old, according to a Statista.com dataset, we’ll want to understand the difference between blood-flow-related vascular dementia and other memory-loss-related conditions.
Vascular dementia vs. Alzheimer’s disease vs. dementia
While some forms of dementia — such as Alzheimer’s disease or Lewy body dementia — are caused by excess protein build-ups and tangles in the brain, vascular dementia is different. Vascular dementia is caused by impaired blood flow to the brain as a result of another condition, such as a stroke.
But, both vascular dementia, Lewy body dementia, and Alzheimer’s progress through several stages that last several years. Medication, occupational therapy, and group activities can be used to help soften the side effects of severe dementia and Alzheimer’s.
The combination of these treatments helps stimulate the brain and keeps the brain active for as long as possible. So, while vascular dementia may develop over several years, a person can live a long, happy, and healthy life with the help of the right treatments, assisted living, and in-home care.
Symptoms of vascular dementia
With all three of these forms of dementia, but especially vascular dementia, a person can experience the following:
- Progressive cognitive decline
- Challenges with making sound judgments
- Communicating and problem-solving
- Memory issues
- Incontinence and trouble swallowing (in late-stage dementia only)
What’s more, people with vascular dementia often encounter mobility problems. Mobility problems occur as a result of damage to the brain caused by decreased blood flow.
Of course, mobility issues don’t always occur. With that being said, certain risk factors predispose individuals to experience mobility problems and vascular dementia as a whole.
Risk factors for being diagnosed with vascular dementia
Those who are most at risk for being diagnosed with vascular dementia include people with the following conditions and health histories:
- Atherosclerosis, a condition that causes arteries to harden
- Health history of cardiovascular and heart disease
- Health history of strokes
The following lifestyle factors can also increase the risk of a dementia diagnosis:
- Smoking
- Excessive alcohol use
- Limited daily exercise
- Being overweight or obese
- Maintaining an unhealthy diet
While there’s no sure-fire way to prevent dementia, living a healthy lifestyle can decrease the chance of damaging blood vessels in the brain thereby reducing the risk of blood clots and other blood-related conditions in the brain that can lead to vascular dementia.
The 7 stages of vascular dementia explained
While scientists haven’t found a way (yet) to prevent dementia, you can help your loved one slow cognitive decline by understanding what’s involved in the seven stages of dementia.
Let’s take a look at each of the vascular dementia stages in greater detail.
Vascular dementia chart: The 7 stages of vascular dementia
1. Typical cognitive behavior/ no cognitive impairment (pre-dementia)
Of the seven stages of vascular dementia, stage one presents the least noticeable symptoms of the seven stages. In this early stage of dementia, dementia patients exhibit normal behavior.
You — and the person with vascular dementia — likely won’t notice the dementia, because the person doesn’t seem to present any visible symptoms.
But, changes in the brain happen in stage one. In other words, though cognitive decline hasn’t yet occurred, early dementia can start years before any symptoms present themselves.
2. Extremely mild cognitive decline (forgetfulness)
In stage two, the first signs of early dementia occur. People with vascular dementia experience general forgetfulness during this stage. Whether a person forgets where they placed items in the house or forgets other details, many people chalk the forgetfulness up to old age.
While mild cognitive decline is common with age, we can’t emphasize enough how crucial checking with your trusted healthcare team is to ensure that this forgetfulness is attributed to old age instead of the onset of early dementia.
3. Mild cognitive decline (increased forgetfulness)
As a person progresses through the seven different stages, mild cognitive decline occurs. While stage three is still considered early-stage dementia, memory loss starts to increase.
For example, in stage three, a person might forget appointments that they made and misplace items around the house. Even so, a dementia diagnosis isn’t always made in stage three because the forgetfulness doesn’t always appear to be dementia-related.
4. Moderate cognitive decline (diagnosis stage)
The fourth stage of vascular dementia is when most people receive a dementia diagnosis. That’s because dementia symptoms become more apparent.
For example, people in stage four may find counting money to be challenging, forget to pay bills, or have a tough time remembering what they ate at their last meal. Stage four dementia tends to last a couple of years.
Yet, vascular dementia progresses at different rates depending on the person. Some people progress to stage five slower than others. In short, every person is different.
5. Moderately severe cognitive decline (day-to-day activities affected)
Stage five dementia is the beginning of late-stage dementia. People with dementia in this stage may struggle with remembering key information.
For example, people with dementia won’t know — or may often forget — their address, phone number, and the appropriate clothing for respective occasions. It’s important to note that most people with dementia in this stage can recall family, friends, and childhood memories.
So, you’ll want to do your best to help slow your loved one’s dementia progression by talking about memories of loved ones. Doing so will help keep your loved one’s brain active during the later stages of vascular dementia.
6. Severe cognitive decline (independent living usually isn’t possible)
Often, at stage six, the progression of the disease makes living at home without help impossible. Many people with vascular dementia rely on care and support teams, assisted living facilities, and memory care in stage six.
Furthermore, behavioral changes may occur. While vascular dementia symptoms vary, we’ve found that at stage six, forgetfulness becomes more commonplace. Also, aggression and anger often occur.
While a person with Alzheimer’s disease or vascular dementia never intends to lose their cool, it’s up to you to remind yourself of this. Whether you’re reminding your 80-year-old loved one to get their steps in each day — or helping them with activities of daily living (ADLs), you’ll want to remind yourself to be patient and compassionate in every interaction.
After all, your loved one needs you most in these final two stages.
7. Very severe cognitive decline (24-hour care needed)
In the final stage of vascular dementia, most people need 24-hour dementia care and supervision. Stage seven of vascular dementia is all about ensuring comfort and quality of life.
While most people with vascular dementia pass away before reaching stage seven due to other health conditions resulting from severe cognitive decline, this stage can last a few years.
New symptoms may present themselves in stage seven, including (but not limited to):
- An inability to speak, move (without much help), chew, swallow, or remember loved ones or caregivers
- Impaired body functions
- Increased time spent sleeping
- Incontinence
While the amount of time a person spends in stage seven is different for each individual, providing quality, comfortable, and compassionate care is crucial in this final stage of vascular dementia.
Did you know?
Did you know November is National Alzheimer’s Disease Awareness Month? Our community takes great pride in not only supporting those battling Alzheimer’s but also raising funds to find a cure.
As an organization, our residents and staff are proud to partner with organizations that have raised over $2,500,000 to support finding a cure. Check out our Facebook page to see what we’ve been up to to support the cure for Alzheimer’s!
Assisted living and memory care solutions for people with vascular dementia
Vascular dementia typically develops over the course of years and through several stages. The seven stages of vascular dementia include:
- Stage one: typical cognitive behavior and no cognitive decline
- Stage two: extremely mild cognitive decline
- Stage three: mild cognitive decline
- Stage four: moderate cognitive decline
- Stage five: moderately severe cognitive decline
- Stage six: severe cognitive decline
- Stage seven: very severe cognitive decline
We know that caring for a loved one with dementia or Alzheimer’s isn’t always easy. At Village Walk, we provide different levels of assisted living for people living with dementia.
If you’re wondering whether assisted living or memory care may be right for you or a loved one, our friendly caregiving team would be happy to answer any questions you have.
Contact us to learn more about assisted living and memory care solutions for people with Alzheimer’s and dementia.
Short on time? You can always browse our comprehensive library of reading materials which includes helpful articles like our quick and comprehensive guide on the pros and cons of assisted living.
We’re here for you if you have any questions, and we look forward to speaking with you soon.
Frequently asked questions (FAQ) about vascular dementia
What types of vascular dementia exist?
Three common types of vascular dementia exist, including:
- Stroke-related dementia: This form of dementia occurs after a stroke occurs or when the blood supply to the brain is impeded due to a blood clot.
- Multi-infarct dementia: This form of dementia occurs after a transient ischemic attack (TIA) — often called a mini-stroke.
- Subcortical vascular dementia: Thought to be one of the most common types of vascular dementia, this form of dementia results because of diseases in the small blood vessels that lie deep inside the brain.
- Mixed dementia: This form of dementia is often caused by a confluence of conditions. Usually, mixed dementia is caused by the combination of Alzheimer’s disease and vascular dementia.
Is vascular dementia treatable?
While no known treatments for vascular dementia exist as of yet, we can slow the progression of dementia and ease the intensity of the symptoms.
With medication, occupational therapy, and group activities aimed at stimulating brain functioning, many dementia patients find their symptoms are more manageable.
What type of care options are available for the different stages of vascular dementia?
Most often, people with dementia and Alzheimer’s can take advantage of the following care options:
- In-home dementia care
- Continuing care boarding communities (CCRCs)
- Assisted living
- Memory care facilities
- Skilled nursing facilities
- Nursing homes
- Other long-term care options
Our reading materials on the differences between memory care and nursing homes and the comparison of assisted living and memory care can shed a bit more light on the differences between the above-mentioned long-term care options.
Otherwise, you’re always more than welcome to reach out by email or phone to speak with our friendly and knowledgeable senior care specialists to learn more.
“All of the staff members go above and beyond…”

“I have nothing but great things to say about this facility. All of the staff members go above and beyond to provide great service for their residents.
Just to name a few: Frank the case manager is so knowledgeable and helpful. The activities organized by Aly are second to none, and the meals prepared by Tom are creative and delicious.
Keep up the good work!” – Christine P., grateful Village Walk partner